The cervix is the entrance to the womb from the vagina and is often described as looking like a pink doughnut in shape and appearance. The pink doughnut is what can be seen when looking at a cervix with a speculum (the instrument used during cervical screening tests) but the cervix is actually tubular and about 3-4cm long. The opening in the centre of the cervix is called the os (the hole in the doughnut).
The inner canal of the cervix is lined with glands that produce secretions throughout your cycle. The consistency of the fluid, and other factors such as the colour and texture indicate the stages of the hormonal cycle and reveals information on your fertility and sexual health. If you are using hormonal contraception such as the pill, an IUD/IUS or the implant your cervical mucous will be thicker.
The cervix itself can be felt inside the vagina, and depending on the day of your cycle may feel firm like the end of your nose, or slightly softer. Depending on where you are in your cycle there will be variations in the position, firmness and angle of your cervix.
How to feel your cervix
Step 1. Wash your hands
Step 2. It will be easier to find if you have one foot raised on a step/ toilet seat. Or lie on your bed with a pillow under your bum to help tilt your pelvis upward.
Step 3. Insert your finger fairly deep into your vagina and you will find your cervix. It should feel firm and tubular, with a small indentation in the middle (the os). You should be able to circle your finger around the edge of your cervix depending on its position.
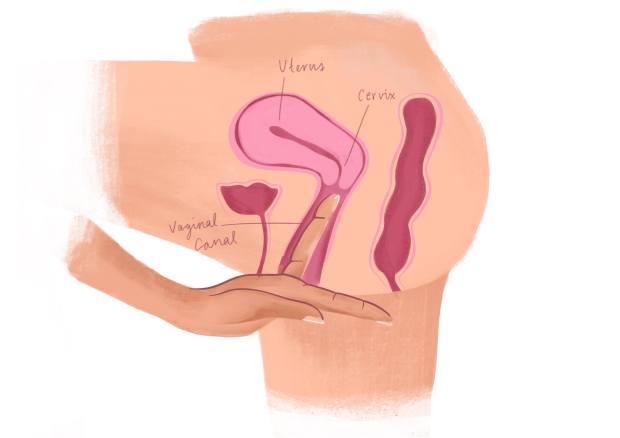
When on your period the cervix will be lower and easier to reach (below left). The os can be felt to be more open, so that your menstrual fluid can be lost easily. When ovulating the cervix will be deeper in the vagina and may be harder to reach (below right). Again, the os will be slightly softer and open. Biologically, this is for the purpose of allowing semen into the cervix more easily in order for ejaculate to make its way to the egg, known as the ovum.

The cervix is constantly producing fluid, and this is responsible for the majority of normal vaginal discharge. After your period finishes, the cervical fluid will be white and sticky. It will then become increasingly runny and watery until ovulation when it begins to resemble a texture like egg white. The fluid becomes stringy and slippery, and can be stretched between your fingers. This illustrates how it assists sperm in swimming up towards the uterus where they will meet an egg, and can also act to preserve the sperm in the vagina. A lecturer of mine literally referred to the fluid as being ‘swimming lanes’ for the sperm!
Why do I need to be able to feel my cervix?
I think it is good to become acquainted with every bit of your body, that is how you will know if something is normal for you or not. Also, if you are using an IUD/IUS as contraception it is important to regularly check that you can feel the strings poking out from the cervix to ensure it is in the correct place. It is possible to monitor your fertility through observing the changes in the cervical fluid combined with other information such as their temperature throughout your cycle.
The website below shows images of a woman’s cervix taken every day of her cycle to show how the cervical fluid and position of the cervix changes. She has not had a baby before or any STIs:
http://beautifulcervix.com/cervix-photo-galleries/photos-of-cervix/
Looking after your cervix
Having regular cervical screening is so important to ensure a healthy cervix. The screening is a method of detecting abnormal cells on the cervix, which are caused by the human papillomavirus (HPV). These cells can be removed before they become cancerous. In the UK screening for cervical cancer starts at 25 years old and is recommended every 3 years until age 49, then every 5 years.
One of the functions of the cervix is to act as a barrier and protect the uterus from infection. The cervix prevents bacteria and viruses that have come into contact with the vagina from infecting the uterus. These organisms can cause inflammation of the cervix, also known as cervicitis. Sexually Transmitted Infections (STIs) are the leading cause of cervicitis.
As a general rule there are two key signs that something is not normal: pain and bleeding. Bleeding between periods and bleeding after sex are abnormal and should always be investigated. Unusual discharge with or without an odour that is yellow, green or grey is also abnormal.
For more information on gynaecological cancers:
https://eveappeal.org.uk/gynaecological-cancers/gynaecological-cancers-brief-explainer/
Glossary:
IUD – Intrauterine device, also known as a copper coil. The IUD is a small T-shaped plastic and copper device inserted into the womb to provide contraception.
IUS – Intrauterine System, also known as the hormonal coil. It is T-shaped device made purely of plastic and releases the hormone progesterone into the womb.
Ovulation – when an egg (ovum) is released from the ovary.